WHEN 1+1=3: HOW ELECTRONIC HEALTH RECORDS AND CLAIMS CAN BE USED SYNERGISTICALLY
April 30, 2015
Sponsored blog posting by DaVita Clinical Research.
1. Combining Drug Development with Real-World Data Analytics
DaVita Clinical Research® (DCR®), a specialty full-service contract research organization, recently merged with HealthCare Partners Clinical Research to further expand its clinical research and data analytics services, specifically in patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD), as well as primary care and chronic disease patients treated in an integrated care organization. The merger resulted in the establishment of longitudinal, de-identified database of 750,000+ multi-specialty patients receiving coordinated, integrated care from HealthCare Partners, and 400,000+ end-stage renal disease patients who have received dialysis during the last five years. With a national laser spotlight on patient-centered disease management combined with the drive to include comparative effectiveness and real-world research in drug development, the approaches used by DaVita Clinical Research offer insight into how a healthcare research organization can marshal multiple resources to inform pharmaceutical research and improve patient outcomes.
HealthEconomics.Com recently interviewed DaVita Clinical Research Medical Director and Vice President, Steven Brunelli, M.D., MSCE, and asked him some questions on how DCR uses both electronic health records and claims data to conduct research.
The combined entity offers access to 750,000+ primary care and multi-specialty patients, as well as 170,000 active dialysis patients, thereby expanding the breadth and depth of the research being conducted.
 |
Patti Peeples (PP)/HealthEconomics.Com: |
For almost two decades, DaVita Clinical Research has focused on kidney-related trials. More recently, your organization has been expanding your access to claims data, electronic health records, as well as patient-reported outcomes data. Why is DCR moving this way?
 |
Steven Brunelli (SB)/DaVita Clinical Research: |
DaVita Clinical Research® is a specialty CRO that began in 1985 as a pharmacology site within an academic hospital, with clinical trial roots in PK studies. Over three decades, the company expanded their focus in renal research to Phase 2 and 3 studies, and then in 2001 added late stage clinical trial capabilities. In 2007, we added a Health Economics and Outcomes Research group, as well as a Real-World Healthcare Data function, and have continued to expand this data analytics portion to gain insight into the longitudinal view of the patient journey through end-stage renal disease.
At the same time, the history of health outcome measures has evolved. A generation ago, the focus was on intermediate values such as A1Cs, hemoglobins, LDLs. Now, there is a much more holistic view of the patient and of outcomes. You don’t hear health systems touting, “we have the best LDL measures.”
The currency of healthcare now encompasses broader outcome measures such as the number of hospitalizations, patient quality of life, or overall survival. We have evolved along with these changes. This latest merger with HealthCare Partners Clinical Research takes us one step further into diseases beyond the renal area into multiple disease states, and provides access to patients and clinical trials conducted within our parent company’s coordinated integrated healthcare system. Our goal is to use our extensive, applied database and real-world healthcare experience to assist in the design, recruitment and completion of retrospective, prospective, pragmatic, and clinical trials. Using these data for informed decision-making however, is not without its challenges and there are some cautionary tales worth mentioning.
[PP] OK, let’s talk about some of these challenges. We now have better and faster access to claims data and patient recorded data; can you describe some of the potential pitfalls or speed bumps with the analyses of claims data?
[SB] There are aspects of administrative claims data that are very strong while some aspects are comparatively weak. For example, certain types of acute episodic events that are clinically overt, like an MI (myocardial infarction), can be fairly well-described by claims data. On the other hand, when trying to describe active or historical patterns of co-morbid disease, or a patient’s underlying risk profile, then claims data are notoriously less reliable.
Recently, we’ve observed here at DaVita Clinical Research that the questions our clients are asking are more nuanced, and this means that we are looking beyond claims data to other sources of information to describe the patient journey.
[PP] What do you mean the research questions to be answered by claims data are more “nuanced”?
[SB] For example, clients are no longer just asking “is the drug effective or ineffective?”, but rather “is this drug effective within a particular subpopulation?”. It’s worth remembering that when more nuanced questions like this are asked, we can get an answer with claims data but it’s not necessarily an accurate answer!
Historically, it wasn’t feasible to do a chart review of 20,000 patients, but an analysis done on a smaller cohort may not yield results that are generalizable to a larger population. It may be feasible to do a much larger administrative claims review, but granularity of detail may be lacking. Additionally, in a typical claims data set the period of enrollment is limited and chronic conditions that are “quiet” in the short term may be missed. In our database the period of enrollment is typically years instead of months, and we also have access to the medical history captured by the physician, providing the granularity that may be absent from claims data.
[PP] Let’s talk about addressing some of these nuances. There is a proliferation of eMobile apps for the patient to track their health data, events, and outcomes. How can these products help researchers and patients in gaining more reliable and accurate data on real-world health events and patient-reported outcomes?
[SB] These apps offer a lot of potential promise, and it’s very exciting as a physician and researcher, but also somewhat troubling. One of the most significant concerns I have as a researcher is the problem of selection bias.
L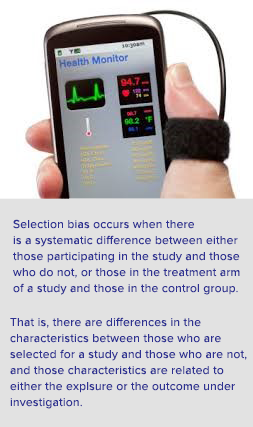
Your readers may be interested in a recently released article describing the software platform, Apple’s ResearchKit, discussing some of the concerns and advantages to using this approach in medical research.
As researchers and healthcare providers, we have to be sensitive to those who are NOT represented in our study sample (often times, it may be the older or poorer patients), and these segments may – in fact – have the greatest need for this data and/or be at the highest risk for health outcomes of interest.
166 million people in the U.S. owned smartphones, as of March, 2014.
[PP] Those are great points. But, do we throw the baby out with the bathwater, or can we address some of these noteworthy challenges like selection bias? How would we get the needed information?
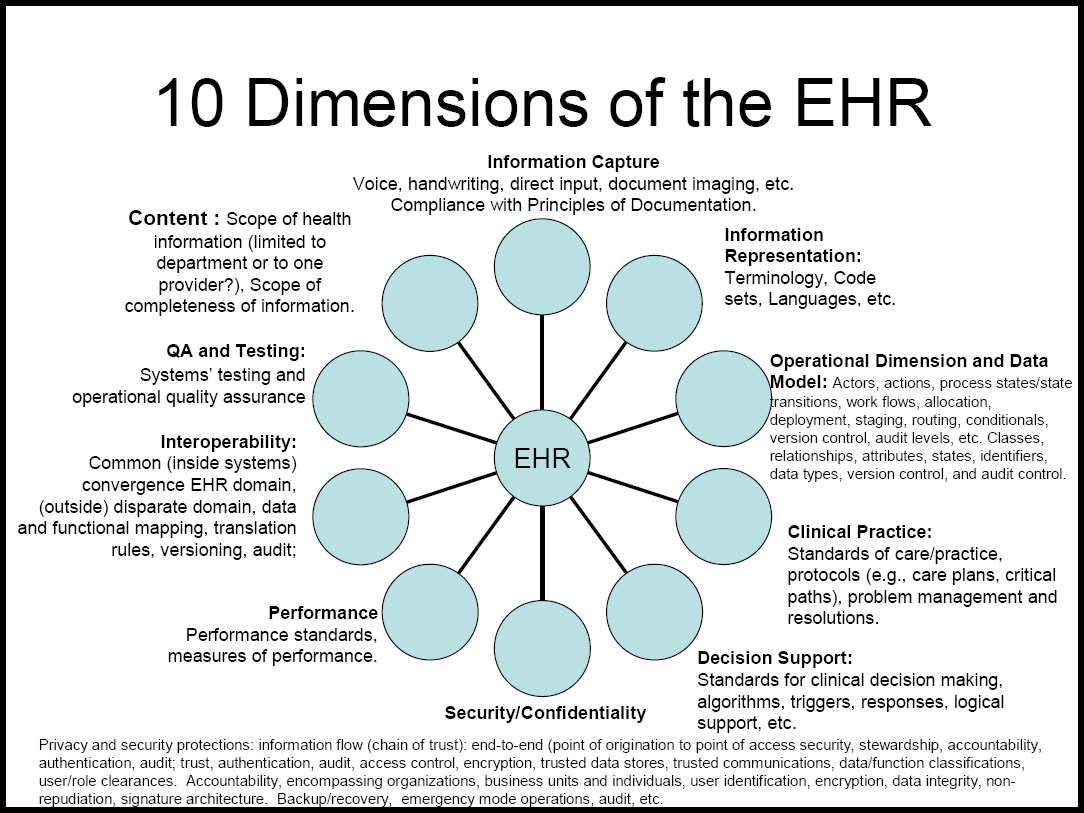
[SB] The goal is to provide similar data on both the 40 year-old iPhone user and the 75 year-old nursing home patient, if they are both relevant to your research question. One has to ask to what extent claims data addresses your concern vs. an eMobile app vs. another resource out there that provides more comprehensive population-level data. One valuable source and tool is electronic health record (EHR) data. EHR data, like all data, are not perfect, but they are much more granular than claims-related data, and EHR data are much less likely to be influenced by implied levels of billing.
[PP] Can you give an example of billing issues and how they would differ with what shows up in claims data vs. EHR data?
[SB] For example, as a physician completing a claim for reimbursement of my professional services delivered during the medical visit, I might select a combination of diagnoses that are relevant to the services I am providing today so that I can be appropriately reimbursed or compensated for my time. Let’s say that the patient had three different medical issues of concern. However, in the process of addressing those three issues with the patient, I might also have identified and noted in my own records that the patient has a number of other health-related problems. Let me give you a more specific example: A nephrologist might write down that a patient has CKD with atrial fibrillation and high blood pressure, and these are the three ICD-9 diagnostic codes noted in the claims and in the EHR. However, in private notes (and in the electronic health record), that nephrologist would also note the patient is on medication for depression and rheumatoid arthritis — much of this detail may be lost on the claims side. For example, if the patient is prescribed lisinopril, the claims data would reflect the filled prescription but the researcher would not know if it was prescribed for heart failure, hypertension, diabetic nephropathy or some combination of those indications. If the patient were taking an OTC med for arthritis that would not be captured. And lastly, if the patient is getting a 90-day supply of prescribed medication, as many health plans require, that may not show up in the short-term. So, within a patient population that has access to EHR data, you aren’t dependent upon the patient self-reporting (which is a downside of mobile apps). And, patients may have many more health-related problems that are considered during a medical visit, and some of these may not be identified or reflected with claims data. However, EHR data allows you to collect both broader (or more complete) standardized data from a broader population, and this increases both the generalizability and the validity of the data.
[PP] Are their drawbacks or limitations to EHR data?
[SB] Certainly! EHR data are very good at recording what is happening for that patient at the time they are seeing the provider who is making the record. A lot of health events occur when they are not seeing a provider. These may or may not be captured in EHR. The doctor may record all medications, procedures, and treatments that they personally provide. However – and this is really important – EHR is also subjected selection bias, in that it reflects that individual provider’s perspective. Another provider might make the same observation and record it differently or not at all. And, EHRs lack the ability to link to other data sources that include death, hospitalizations, prescription or non-prescription behavior, and care by other providers, as well as what I mentioned before – health events that occur when not in the presence of a healthcare provider.
2. Benefits of a Provider-based Organization
[PP] Why don’t more of the contemporary analyses utilize both claims and medical records data?
[SB] In a recent project with a client, the client was interested in understanding the burden of anemia in the population, including the treatment options and effectiveness. They wanted to assess how those treatments related to subsequent outcomes. To understand the need for combined data sources, you have to be able to differentiate whether the manifestation of anemia is primary (e.g., related to a disease like sickle cell, etc.) or either brought on or further exacerbated by chronic or acute conditions (that is, secondary anemia). Therefore, to really understand how the treatment choices were made, one needs to under the entire disease burden and medical spectrum of the individual patient. Using our proprietary HCP database, consisting of integrated EHR data, lab values, and pharmacy and medical claims data on approximately 750,000 members receiving integrated care, we were able to identify all the acute and chronic conditions that beset patients and also gain a detailed understanding of associated demographic characteristics of those patients in our database. We were able to, on the claims side, identify medical treatments that were rendered in response to the anemia and understand the effect of those treatments on the anemia itself by bringing back in the laboratory data from the EHR side. This closed the loop and helped us understand how all of these factors may have had an impact upon healthcare utilization and economics such as hospitalizations (provided in the claims data). So, this gave us a strong proof-of-principal of the benefit of combining two data sources, EHR and claims, and directly linking patient experience to gain a more comprehensive understanding of the disease.
[PP] Thank you for giving us some real-world examples of the use of secondary data like claims and electronic health records can be used to reflect patient care and outcomes. For more information on the DaVita Clinical Research® approaches to real-world and late phase research, as well as data analytics, visit their website at: http://www.davitaclinicalresearch.com/. DCR® has a scientific library providing their publications and research presentations, available at http://www.davitaclinicalresearch.com/media-library/scientific-library/ .
Disclosure: The contents of this blog posting are submitted and paid for by DaVita Clinical Research®,
a wholly owned subsidiary of DaVita Healthcare Partners, Inc.