Advancing Real-World Evidence with Pragmatic Clinical Trials: Interview with Dr. Joseph Singer, Chief Medical Officer of HealthCore-NERI
January 21, 2019
Dr. Patti Peeples, CEO of HealthEconomics.Com, sat down with Dr. Joseph Singer, CMO of HealthCore-NERI, to discuss how pragmatic clinical trials are advancing real-world evidence (RWE). The mission of HealthCore-NERI is to provide clarity that empowers decision makers to act with precision to improve quality, safety, and affordability in healthcare. HealthCore-NERI works with life science companies, payers and providers, and government and academic organizations to provide real-world evidence in support of a wide variety of healthcare decisions.

Dr. Peeples: What is the shift we are seeing in the industry from typical Randomized Controlled Trials (RCTs) design to Pragmatic Clinical Trials (PCTs) design?
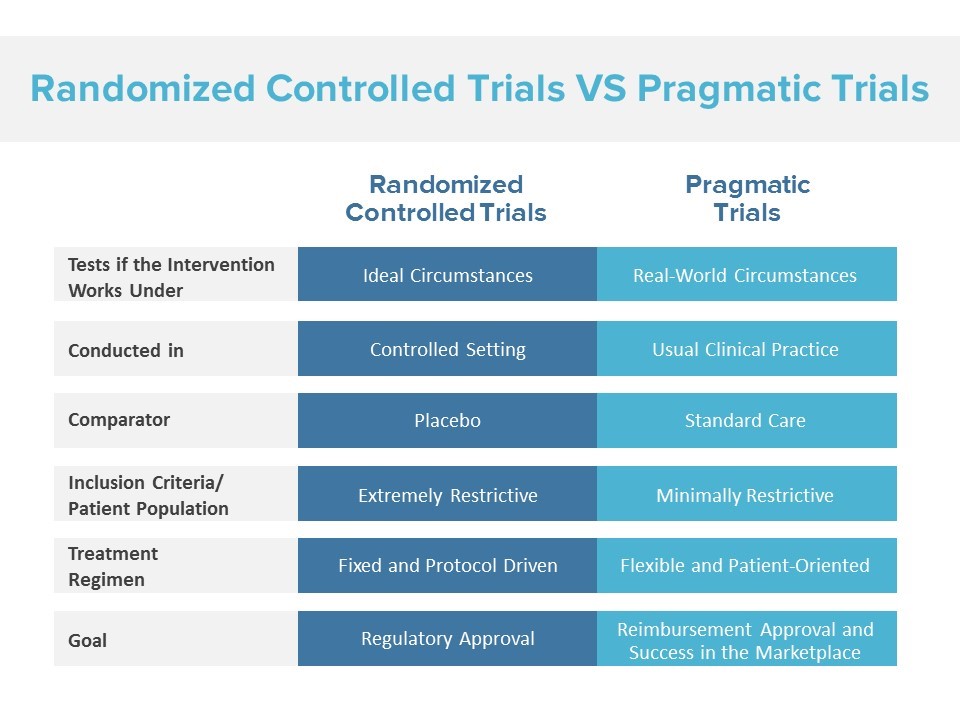
Dr. Singer: For the past fifty years, healthcare has been relying on randomized controlled trials (RCTs) to establish safety and efficacy of medical and surgical treatments. RCTs have been integral in establishing the potential efficacy and the beginning of understanding the risk profiles of new treatments and interventions. While RCTs have been the standard for evaluating early phase therapies, they are limited in evaluating treatment options in a real-world, post-approval setting. Real-world evidence using pragmatic clinical trials (PCTs) is increasingly being used for decision making by payers, life science companies, health systems, and practicing physicians. There is a need for devices and interventions, both biopharmaceutical and surgical, in a value-based system to demonstrate the actual benefit and risks occurring in a real-world patient setting, as opposed to the tightly controlled populations of a traditional RCT. Pragmatic studies allow for observation of a more generalizable and diverse population, and are designed to include many different kinds of patients – with various comorbidities, ages, and demographics. We have seen a strong industry shift toward these new types of studies with the PDUFA VI Regulations and the 21st Century Cures Act, requiring the FDA to explore the use of real-world evidence in support of new indications for approved drugs or fulfill post-approval requirements. There is significant potential gain by integrating results of both efficacy from RCTs and effectiveness from PCTs to personalize most appropriate placement of an intervention in the treatment plan of individuals by their treating physicians.
Dr. Peeples: How are Pragmatic Clinical Trials advancing Real World Evidence?
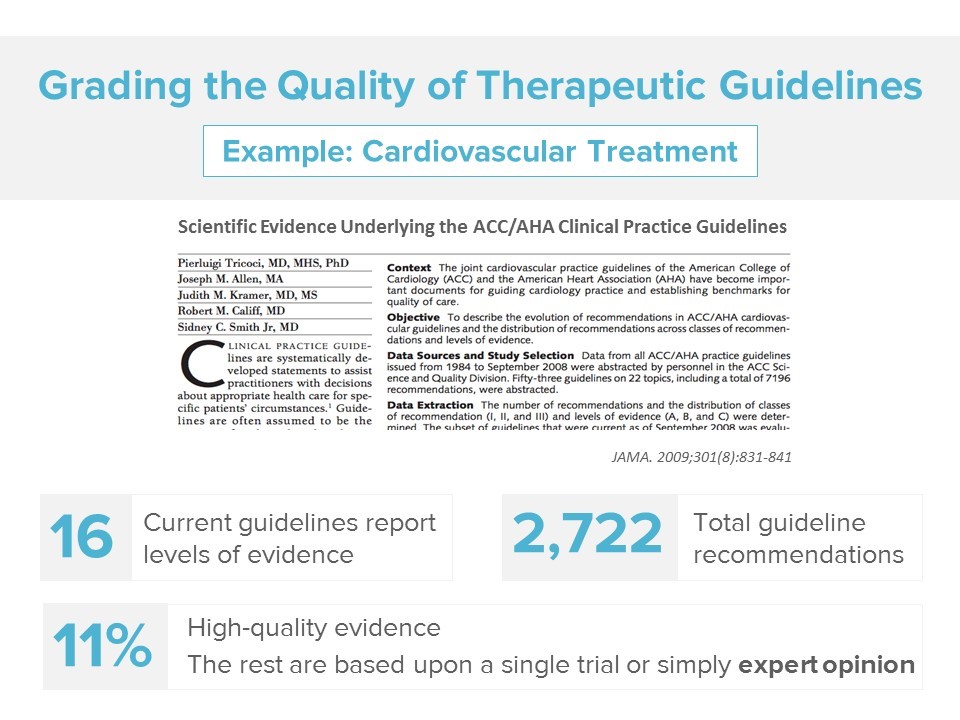
Dr. Singer: Currently, as little as 15 percent of clinical guidelines are based on solid evidence. For instance, if we zero in on cardiovascular guidelines, there are 16 high impact cardiovascular guidelines used to power healthcare decisions by payers, healthcare providers and consumers – with 2,722 recommendations within these guidelines. However, only 11 percent are actually based on enough evidence to warrant the recommendation, with most only relying on a single trial or expert opinion.[1] Expert opinion is essential to fill gaps in evidence when strong scientific evidence has not been generated, but it is not optimal for personalizing care for any given patient.
One way to get at generating real-world evidence is through retrospective research looking at utilization and costs, but another important way to study real-world evidence is through prospective study designs that randomize patients to various treatment options to determine the appropriate treatment for patients in the real world. PCTs enable the healthcare industry to more nimbly and efficiently answer questions related to how a treatment option performs in a real-world setting, contributing important evidence to establish future clinical guidelines that are applicable to a broad array of patients.
Dr. Peeples: What are the benefits to Pragmatic Clinical Trial design?
Dr. Singer: While retrospective research can answer important questions about trends and utilization of certain treatment options, prospective study designs allow us to more accurately observe treatment effects because of randomization. However, traditional prospective study designs, such as RCTs, offer challenges in terms of implementation and often don’t include a representative patient population.We know that over90 percent of patients do not participate in traditional RCT research. An important contributing factor is the overall burden, time and resources required of participating physicians and patients in these complex and highly structured studies. Because pragmatic clinical trials are rooted in real-world practice, they require significantly less time and resources. Physicians do not need to take hours on a daily basis to document findings, to hire additional staff and disrupt their typical practice operational flow. Often times, patients’ participation in the trial only requires informed consent, randomization and responding to a few surveys. Therefore, it opens the door to include many more physicians for participation and offers opportunities for their patients, which ultimately improves our understanding of how treatments perform in routine practice.
PCTs are designed to be minimally burdensome to both participating physicians and patients, are structured to allow existing office staff to do much of the work, and minimize the bureaucracy and paperwork associated with performing research.
Dr. Peeples: What are some of the challenges with implementing PCTs?
Dr. Singer: Moving from high-touch research interventions to real-world pragmatic studies requires a complete shift in mindset among the FDA, the industry, trial sponsors and trial participants. What works in RCT implementation may not work in PCT implementation. Rather than targeting the same traditional physician groups, who offer a limited number of patients, there is an opportunity to work with more research limited or research naïve sites. Working with these sites does pose some challenges, such as provider and patient unfamiliarity with research and limited staff support and resources. However, the lean resource approach PCTs can take allows seamless integration with community clinics who may lack experience with research but who have the ideal patient population for implementation.
Dr. Peeples: How can we overcome barriers to physician and patient recruitment?
Dr. Singer: We recognize that85 percent of RCTs fail to meet recruitment targets, with 15 to 20 percent of trial sites never enrolling a single patient.[2,3] To meet and exceed targets and timelines, a new set of tools is needed to address physician and patient recruitment into PCTs. First, it is essential to know the ideal physicians and sites to target and approach. Secondly, sites need the appropriate tools and resources to identify and enroll patients, and conduct the research. Through the use of site intelligence (physician and patient population demographics), targeted physician and patient communications, and technology automation, PCTs can improve efficiency, meet enrollment targets and exceed timelines.
Dr. Peeples: What is the best way to get started on designing and implementing a PCT?
Dr. Singer: Success for PCTs involves an understanding of the unique challenges of pragmatic studies, and having the right tools to overcome those barriers. At HealthCore-NERI, through the Integrated Research Network (IRN), a connected network of physicians, integrated delivery systems, patients and payers, we are building the ecosystem to support real-world evidence, pragmatic clinical trials. The IRN uses a unique identification and automation processor to leverage existing relationships and intelligence collected on sites to accelerate time to first patient in. Through targeted communications, we equip sites with the tools they need to be successful in patient recruitment. We’ve created a community where physicians and patients become the direct recipients of the research we conduct to improve quality and satisfaction and to foster long-term engagement.
Dr. Peeples: Thank you, Joe. For more information on the Integrated Research Network (IRN), pragmatic clinical trials, and other HealthCore-NERI research solutions, contact IRN@HealthCore.com.
[1] Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC Jr. Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA. 2009; 301:831–41. Available here: https://jamanetwork.com/journals/jama/fullarticle/183453
[2] Carlisle B, Kimmelman J, Ramsay T, MacKinnon N. Unsuccessful trial accrual and human subjects protections: an empirical analysis of recently closed trials. Clin Trials 2015; 12:77-83. Available here: https://journals.sagepub.com/doi/abs/10.1177/1740774514558307?journalCode=ctja
[3] Budgeting at the Investigative Site, University of North Carolina at Chapel Hill, Office of Clinical Trials Newsletter. July/August 2006.

Dr. Joseph Singer is responsible for guiding HealthCore-NERI’s project teams to optimize the clinical, coding, and insurance industry perspectives embedded within their analytic projects. He also supports development of clinical aspects of HealthCore-NERI’s research environment and manages HealthCore-NERI’s Integrated Research Network (IRN). As an Initiative Owner, he is leading the development of a research environment to optimize the efficiency and effectiveness of studies performed by HealthCore-NERI. He serves as clinical lead for several Payment Innovation activities within Anthem, Inc. (i.e. building the bundled payment methodologies), as well as provides leadership in numerous enterprise steering committees






