COVID-19 and Racial/Ethnic Disparities in Health
February 4, 2021
April M. Falconi, PhD, MPH
Senior Researcher, Population Health, Translational Research
HealthCore, Inc.
The COVID-19 pandemic has been characterized by surges in infections in different parts of the country at different times. The most recent rebound of COVID cases, however, indicates that the COVID-19 pandemic is not just a series of isolated surges that is “one and done.” It is more of an ebb and flow of transmission that has had and will continue to have a profound effect on all people, even after the vaccine has been distributed.
Although COVID-19 is highly infectious and is easily spread regardless of race, education, or income level, racial and ethnic disparities in disease prevalence and mortality have persisted. Our findings on racial and ethnic inequities in COVID-19 represent one of few studies that uses data from a diverse population collected from a large, national insurer that covers millions of lives across all 50 states. The added contribution of our analysis lies in offering a perspective gleaned from a different data source and from a geographically diverse population.
Racial and Ethnic COVID-19 Inequities: Testing, Hospitalizations, and Deaths
Our analyses of a commercially-insured population show that Black and Hispanic/Latino populations appear more likely to test positive for COVID, to be hospitalized for COVID, and to die from COVID in the hospital, relative to White and Asian populations. These disparities are exacerbated in certain age groups—particularly those who are in their prime working-age years.
The pervasiveness of racial and ethnic disparities in COVID infections and outcomes emanates from a history of social inequities and racial disparities in healthcare1 and are attributable to two factors: 1) racial/ethnic minority populations are at higher risk for infection due to the environments in which they live and work2, and 2) ethnic minority populations are more likely to have underlying conditions resulting in more serious disease outcomes from COVID (e.g., hospitalization, admission to an intensive care unit, death)3.
Our analyses are based on only those individuals who provided race and ethnicity data (approximately 30 percent of the 35 million lives covered in our analyses). We note, however, the issue of missing race and ethnicity data is not unique to our dataset, as race/ethnicity data has routinely not been collected during the commercial health plan enrollment process4. Similarly, published state and county-level race and ethnicity data on COVID infections remains limited despite improved data collection and reporting over the past several months.
Due to the time lag required to process claims and ensure data accuracy, our analyses of commercial health plan members encompass data between January and August 2020 (unless otherwise noted).
Black and Hispanic/Latino Populations More Likely to Test Positive for COVID-19
Among those who were tested for COVID, the Black and Hispanic/Latino populations showed the highest likelihood of testing positive (see Figure 1). Between January and July 15, 2020, the Black population showed a 8.2 percent test positivity rate, while the Hispanic/Latino population showed a 7.4 percent test positivity rate, compared to the White and Asian populations who showed 5.4 percent and 4.2 percent test positivity rates, respectively.
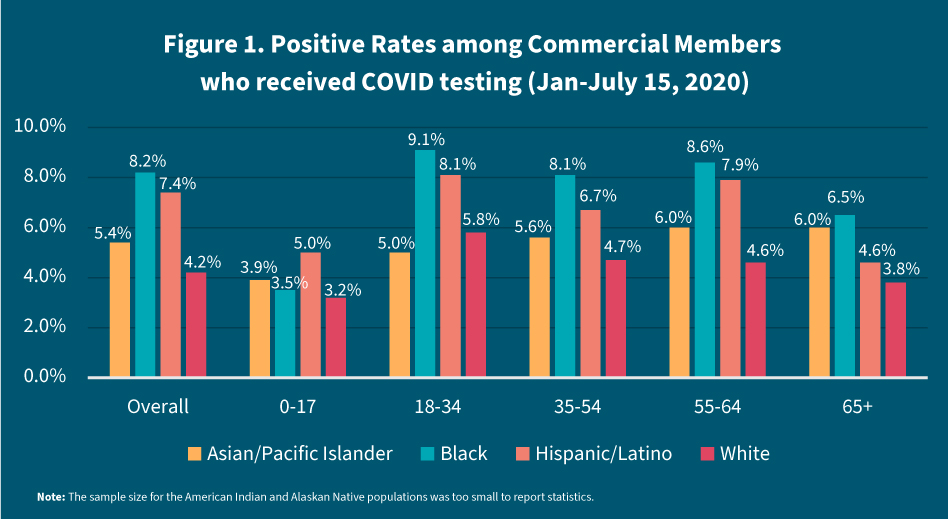
A test positivity rate reflects the probability that a tested individual will receive a positive result. A higher percent positivity rate suggests the group is experiencing relatively higher disease transmission among minorities, and it also indicates lower access to testing. High test positivity rates can occur when only those who are worried they might be sick are tested. Low test positivity rates can occur when tests are administered to many people, including those who are unaware they are at risk. When more non-COVID cases are included among those who are tested, the test positivity rate declines.
Work and Home Environments Contribute to Racial and Ethnic Minority Populations’ High Test Positivity Rates
Racial and ethnic minorities have a greater risk of disease exposure because they are more likely to work in jobs considered “essential” or “frontline,” such as in healthcare facilities, grocery stores, construction, or factories, and are more likely to take public transportation to get to their jobs. Black and Hispanic/Latino populations also are more likely to live in densely populated neighborhoods and in shared living or housing environments, where personal space is limited and inhibits quarantining as needed. No matter how diligent or cautious their preventive behaviors are taken (e.g., handwashing, wearing a mask, social distancing in public), they are less able to avoid infection.
Racial and Ethnic Minority Populations More Likely to be Hospitalized from COVID-19
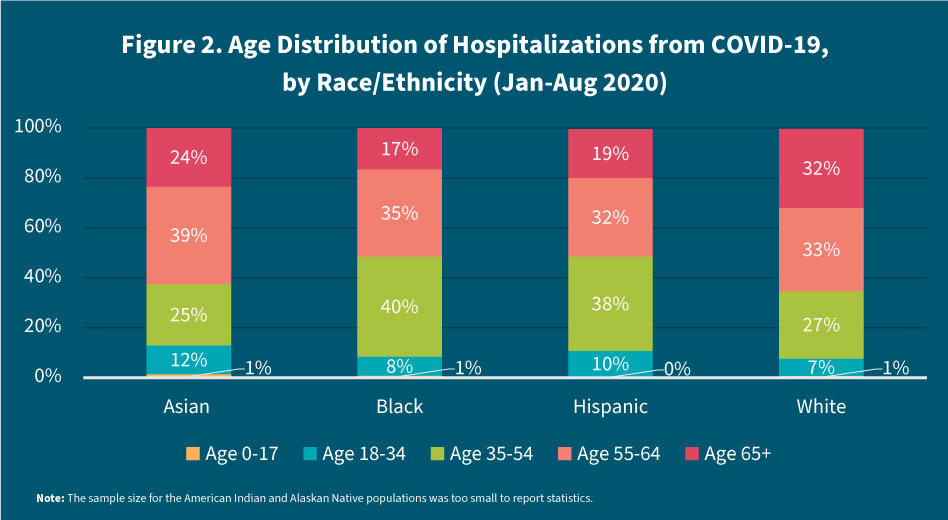
The Asian, Hispanic/Latino, and Black populations who test positive for COVID are more likely to be hospitalized at younger ages compared to the White population—especially the Hispanic/Latino and Black populations. While more than one-third of all COVID cases occur in the 35-54 age group— contributing to the large proportion of hospitalizations that occur during these ages across all races, the share of hospitalizations occurring in the Black and Hispanic/Latino populations is disproportionately high. Roughly 75 percent of hospitalizations in the Black population occur among adults in their prime working-age years, including 40 percent among individuals ages 35 to 54 and 35 percent among individuals ages 55 to 64. Similarly, 70 percent of hospitalizations in the Hispanic/Latino population occur in their prime working-age years – 38 percent for ages 35 to 54 and 32 percent for ages 55 to 64 (see Figure 2).
Death
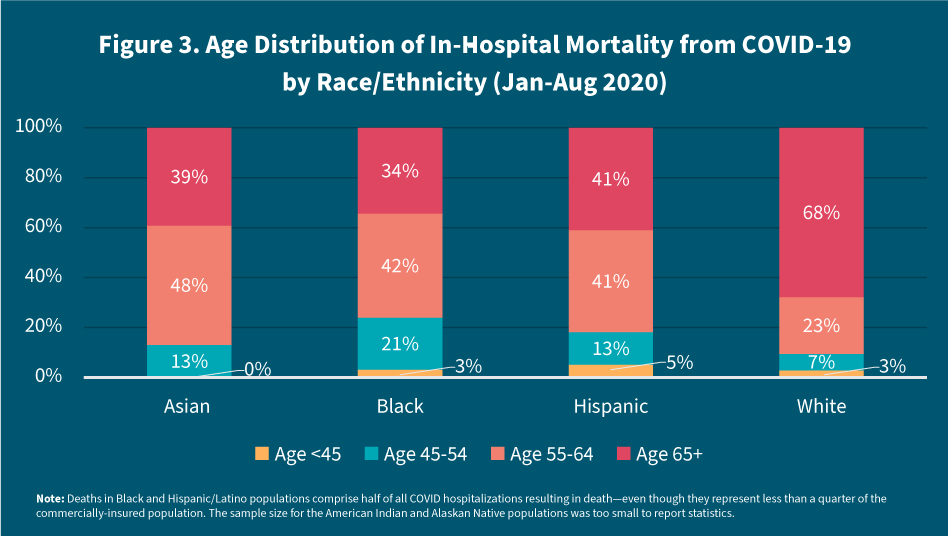
Across all age groups, the Hispanic/Latino population represents more than a third, or 38 percent, of COVID hospitalizations resulting in death among the commercially-insured, despite accounting for only 11 percent of the commercially insured population. As many as 12 percent of COVID hospitalizations (across all racial/ethnic groups) resulted in death among the Black commercially insured population, even though only 9 percent of commercially-insured enrollees identify as Black. Less than half, or 47 percent, of all COVID hospitalizations resulted in death among the White commercially-insured population, despite their accounting for 55 percent of the commercially-insured population.
While deaths appear clustered at ages 65 years and older for the White population, the majority of deaths are spread across the relatively younger age groups in the Hispanic/Latino and Black populations. For example, 63 percent of deaths from COVID in the Black population occur between the ages of 45 and 64, while 54 percent of deaths from COVID in the Hispanic/Latino population occur between the ages of 45 and 64. Only 30 percent of deaths in the White population, in contrast, occur among this age group (see Figure 3).
Black and Hispanic/Latino Populations’ Underlying Conditions Contribute to Serious Outcomes from COVID-19
Racial and ethnic disparities in health begin at birth5,6, and persist over the life course, regardless of an individual’s level of education, income, neighborhood, or access to healthcare7. Black and Hispanic/Latino populations, consequently, are more likely to experience serious outcomes, such as hospitalization or death, from COVID-19 due to minority populations’ relatively higher prevalence of underlying conditions, including stroke, diabetes, and kidney disease. The Black population also has shown higher rates of cancer relative to the White population8,9. All of these conditions have been found associated with increased likelihood of hospitalizations or mortality from COVID-19. Prior research also has shown providers’ implicit biases (i.e., thoughts and feelings outside of conscious awareness) are associated with health outcomes10 and may further contribute to inequities in COVID-outcomes among minority populations.
What can be done?
Racial and ethnic disparities in COVID-19 must be addressed if we wish to rein in the pandemic in the United States. Healthcare payors can be an integral part of the solution by working to reduce racial/ethnic disparities in the testing, treatment, and vaccinations (as they become available) for COVID-19. Payors should work directly with trusted community leaders and organizations (e.g. churches, neighborhood groups/centers) to provide member outreach and information on COVID prevention, testing, and vaccinations. Testing sites, for example, need to be located at easily accessible and familiar locations throughout communities and with longer operating hours (e.g. after working hours). Communications and educational materials need to clearly state there is no charge for testing or for the vaccine, as required by government regulations.
Treatment can be made more available by improving access to telehealth and through eliminating patients’ out-of-pocket costs for receiving COVID treatment. Structural barriers, such as limited access to broadband internet services and financial burden, have historically impeded utilization of telehealth services among Black and Hispanic populations. Waiving copays for telehealth visits would help remove a financial barrier, but minority communities must also be made aware of benefit changes. Although many plans have waived out-of-pocket payments for COVID treatment and telehealth visits, lack of awareness of these services at no cost continues to delay seeking care.
Lastly, in order to encourage widespread vaccination, the COVID-19 vaccine should be made available at convenient, easily accessible locations. People need to be made aware, moreover, that the vaccination is free of charge, as required by law. Reducing geographic and financial barriers is important, because another hurdle that needs to be addressed is increasing the trust of racial/ethnic minority populations in the healthcare system. Survey data indicate, for example, that Black adults are the least likely to indicate they would get a COVID-19 vaccine11; similarly, research shows that distrust and safety concerns contribute to disparities in other vaccination rates, such as for flu12. The documented issue of distrust in the healthcare system by minority groups, especially the Black population, can be addressed by healthcare payors through devoting resources toward the financing of initiatives to reduce disparities in healthcare. Local community health organizations may also serve as a bridge that helps to build trust in the healthcare system among the racial and ethnic minorities.
We hope the findings from these analyses illuminate the broader issue of racial and ethnic inequities in health and help advance long-overdue changes to create a better future for all. At HealthCore, we are committed to taking an evidence-based approach to inform strategies aimed at providing equitable care and driving optimal health outcomes for our communities.
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. UNDERSTANDING AND ELIMINATING RACIAL AND ETHNIC DISPARITIES IN HEALTH CARE, BACKGROUND PAPER RACIAL AND ETHNIC DISPARITIES IN HEALTH CARE: A BACKGROUND AND HISTORY. Available from: https://www.ncbi.nlm.nih.gov/books/NBK220343/
- Selden TM & Berdahl TA. (2020) “COVID-19 and racial/ethnic disparities in health risk, employment, and household composition.” Health Affairs; 39:1624-1632.
- Gu T, Mack JA, Salvatore M. (2020). “Characteristics associated with racial/ethnic disparities in COVID outcomes in an academic health system.” JAMA Network Open; 3(10):e2025197.
- Escarce JJ, Carreon R, Veselovskiy G, Lawson EH. (2011). “Collection of race and ethnicity data by health plans has grown substantially, but opportunities remain to expand efforts.” Health Affairs, 10:1984-1991.
- Keating, K et al. (2020). “Maternal and Child Health Inequities Emerge Even Before Birth.” State of Babies Yearbook 2020. Child Trends. Available at https://stateofbabies.org/wp-content/uploads/2020/06/Maternal-and-Child-Health-Inequities-Emerge-Even-Before-Birth.pdf. Accessed November 9, 2020.
- Lu, MC and Halfon N. (2003) “Racial and Ethnic Disparities in Birth Outcomes: A Life-Course Perspective.” Maternal and Child Health, 7:13-30.
- Williams DR, Lawrence JA, Davis BA. (2019). “Racism and Health: Evidence and Needed Research.” Annual Review of Public Health, 40:105-125.
- Gansevoort RT and Hilbrands LB. (2020). “CKD is a key risk factor for COVID-19 mortality.” Nature Reviews Nephrology. 16:705-706.
- Li Q et al. (2020) “Cancer increases risk of in-hospital death from COVID-19 in persons <65 years and those not in complete remission.” Leukemia, 34:2384-2391.
- Hall WJ et al. (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health; 105:e60-e76.
- Tyson A, Johnson C, Funk C. U.S. Public Now Divided Over Whether to Get COVID-19 Vaccine. September 17, 2020. Pew Research. Available at https://www.pewresearch.org/science/2020/09/17/u-s-public-now-divided-over-whether-to-get-covid-19-vaccine/. Accessed December 4, 2020.
- Quinn SC. (2018) African American adults and seasonal influenza vaccination: Changing our approach can move the needle. Human Vaccines & Immunotherapeutics; 14:719-723.








